Quality Focus
It is important to us that you experience quality health care and customer service. Your satisfaction matters to us. The Quality Management (QM) program ensures our services meet high standards of quality and safety. We want to make sure you have:
- The right kind of care
- Easy access to quality medical and behavioral health care
- Help with any chronic conditions or illnesses
- Support when you need it most
- High satisfaction with your doctors and with us
Quality Management Program
RCBP’s Quality Management Program works to ensure that all of our services meet high standards of quality and safety. We have quality programs so that you can get the care you need. Some of our quality programs are:
- Surveying members and providers to measure satisfaction
- Calling members to remind them to get their care
- Educating members by sending postcards or newsletters
- Reviewing the type, amount and quality of services given to members
- Working with members who have chronic health issues through case management
- Reminding providers and members about preventive health care
- Measuring standards like how long it takes for a member to get an appointment
- Monitoring phone calls to make sure your call is answered as quickly as possible and that you get correct information
- Reviewing calls and complaints from members
- Reviewing all aspects of the health plan with health plan staff, providers and members through various steering committees
If you have a concern or want to learn more about our quality programs, please call Member Services at 1-800-638-8432.

HEDIS® and CAHPS® Performance Results
RCBP is committed to improving clinical outcomes and member satisfaction with the health plan. The Healthcare Effectiveness Data and Information Set (HEDIS) and Consumer Assessment of Healthcare Providers and Systems (CAHPS) are a set of performance measures that help us to see how well we perform.
What is HEDIS®?
HEDIS is a tool that measures performance in the delivery of medical care and preventive health services. HEDIS® is coordinated and administered by NCQA (National Committee for Quality Assurance) and used by the Office of Personnel Management (OPM) for monitoring health plan performance.
Why is HEDIS® important?
Health plans use HEDIS® results to measure performance, pinpoint quality initiatives, and deliver educational programs for members and providers. HEDIS® evaluates both physical and behavioral health clinical practice guidelines (CPG) adherence and provides a consistent way to evaluate the quality of care provided to our members.
RCBP’s 2023 results based on NCQA percentile benchmarks*:
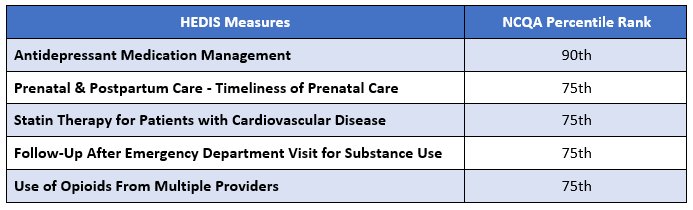
*Percentile data is taken from the NCQA Quality Compass® Benchmark and Compare Quality Data using ALOB (All Lines of Business) benchmarks.
What is CAHPS?
CAHPS is an annual survey which is used for rating a patient’s health care experiences when navigating the health care system. The survey asks patients to report on their experiences with health care services in different settings.
How can RCBP serve you better?
The CAHPS survey gives you the chance to tell us what you think about the services we provide at RCBP. Annually, the survey will be mailed to about 1,100 randomly selected health plan members. Your submission remains confidential with the third-party administrator of the CAHPS survey. If you receive the survey in the mail, it is very important that you fill it out and return it right away. Thank you for helping to make our members’ experience better.
The CAHPS Survey will help RCBP:
- Identify areas that cause member dissatisfaction
- Develop lasting quality improvement initiatives
- Report survey outcomes confidentially to OPM
Why is CAHPS important?
It empowers prospective members to benefit from the experience of others. Patient experience surveys focus on asking patients whether or how often they experienced critical aspects of health care, including network adequacy and availability, communication with their doctors, understanding their medication instructions, and the coordination of their healthcare needs. Positive patient care experiences also relate to key aspects of the perceived quality of care and to clinical outcomes, as patients are more engaged and adherent to the recommended plan of care.
If you ever receive a survey, please take the time to complete it. We will continue to work hard to offer you great health care and best in class customer service.
RCBP’s 2023 results based on NCQA percentile benchmarks*:
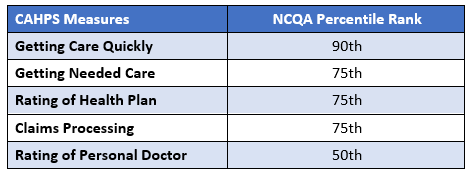
*Percentile data is taken from the NCQA Quality Compass® Benchmark and Compare Quality Data using ALOB (All Lines of Business) benchmarks.
Provider Satisfaction with Utilization Management
RCBP is committed to improving provider satisfaction with the health plan. To assess our provider satisfaction, data collected from internally administered satisfaction surveys are used to analyze and identify opportunities for improving provider satisfaction. The satisfaction survey is offered to providers through an interactive voice response system (IVR). The provider may voluntarily complete the survey over the phone after the health plan representative concludes the call. The data is evaluated and presented to the Quality Improvement Committee at least annually.
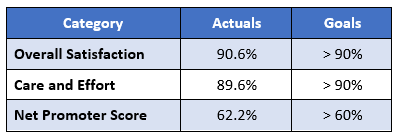
2023 Provider Satisfaction Results: